The Human Need for Salt
| “In all ages salt has been invested with a significance far exceeding that inherent in its natural properties…Homer calls it a divine substance. Plato describes it as especially near to the gods, and we shall presently note the importance attached to it in religious ceremonies, covenants and magical charms. That this should have been so in all parts of the world and in all times shows that we are dealing with a general human tendency and not with any local custom circumstance or notion.” Ernest Jones, 1912 |
Salt has been a highly prized substance for thousands of years across all cultures and continents. Yet over the past few decades, excess salt and sodium intake has been blamed for a variety of serious health conditions plaguing our country, such as heart disease, hypertension, and stroke.
Much debate has centred around determining the level of dietary salt required to maintain optimal health, but over the years the suggested upper limit has continued to shrink. According to the CDC, the average intake of sodium for American adults is about 3,300 mg of sodium a day, which is well above the standard recommendations. The USDA urges Americans to consume less than 2,300 mg of sodium per day, and the American Heart Association (AHA) has an even more strict guideline of consuming less than 1,500 mg a day for general health and disease prevention.
It has been theorized that dietary salt consumption was extremely low in the Palaeolithic diet – approximately 768 mg of sodium daily – and that inland hunter-gatherers added little or no salt to their food on a regular basis. We know these hunter-gatherer diets did not lead to the chronic, Western diseases we see today. The question is, does low salt intake by our distant ancestors mean that adding salt to our food is necessarily harmful? Should we adhere to the AHA sodium guidelines of 1,500 mg or less per day? Or is there a healthy range of salt consumption that can not only support but optimize our health?
Physiological roles of salt in the human body
Despite its recent bad press, there is no doubt that an adequate intake of salt in the human diet is required to maintain good health. The Institute of Medicine recommends that healthy adults consume 1500 mg of sodium, or 3.8 grams of salt, to replace the amount lost daily on average through sweat and urination. (Ironically, this recommendation is almost double the amount theoretically consumed by Palaeolithic man.) The minimum physiological requirement of sodium simply to sustain life has been estimated to be 500 mg of sodium per day.
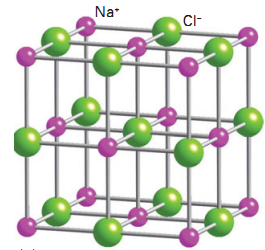
Sodium is a vital nutrient. It’s a major component of extracellular fluid, and is essential for maintaining the volume of the plasma to allow adequate tissue perfusion and normal cellular metabolism. Because sodium is used as an extracellular cation, it is typically found in the blood and lymph fluid. The maintenance of extracellular fluid volume is an important physiologic function of the sodium in the body, particularly in regards to cardiovascular health.
Besides helping to maintain fluid balance and cardiovascular function, sodium and chloride ions also play an important role in the nervous system. Changes in the concentrations of these ions allow neurons to send signals to other neurons and cells, allowing for nerve transmission as well as mechanical movement. Chloride ions provided by salt are secreted in the gastric juice as hydrochloric acid (HCL). And HCL is vital to the digestion of food and the destruction of food-borne pathogens in the stomach.
If a true sodium deficiency occurs, mammals experience symptoms of hyponatremia such as brain swelling, coma, congestive heart failure, cardiovascular collapse following acute blood loss, and impaired sympathetic cardiovascular adjustments to stress. Animals in a truly sodium-deficient state will seek out salty food and often consume far more sodium than needed to restore homeostasis. These behavioural changes in response to inadequate salt intake further demonstrate the biological importance of dietary salt.
Regulation of plasma sodium levels by the kidney
The kidney, when healthy, regulates sodium and water excretion using hemodynamic, neural, and hormonal inputs. This allows it to respond appropriately to a wide range of dietary sodium intake. Aldosterone, a steroid hormone secreted by the adrenal glands, helps regulate the balance of water and electrolytes in the body.
An abrupt increase in dietary salt can cause a redistribution of fluid from the intra- to the extracellular space. But after a few days, the kidney is able to compensate with extra sodium excretion to match the dietary intake. Therefore, healthy people are generally able to adapt to a wide range of salt intakes without a significant change in blood pressure.
If sodium intake drops too low, our metabolism shifts into a sodium-sparing mode. This stimulates the renin-angiotensin-aldosterone hormonal system, which in turn maintains osmotic balance and adequate blood pressure. A significant increase in renin and aldosterone is a symptom of sodium insufficiency, and has been shown to occur as salt intake drops below 1.5 teaspoons per day. Interestingly enough, the recommendation for 2,300 mg of sodium equates to approximately one teaspoon of salt. An intake this low is associated with an even more rapid rise in renin.
Another important dietary determinant of this renin-angiotensin-aldosterone hormonal system is potassium intake. Our biological machinery (which developed in the Palaeolithic era) evolved in conjunction with a diet not only very low in sodium, but also very high in potassium-rich plant foods. Unlike our Palaeolithic ancestors, Americans are consuming very low amounts of potassium: approximately 3,200 mg per day in men and 2,400 mg per day in women. The adequate intake as defined by the IOM is 4,700 mg per day, and pre-agricultural humans are estimated to have consumed fully 10,500 mg of potassium each day.
This modern reversal of electrolyte consumption is another important consideration in determining the population-wide increase in rates of hypertension. Dietary potassium has been demonstrated to dose-dependently counter the pathophysiological effects associated with modern dietary excess of salt, including salt-sensitivity, a likely precursor of hypertension. Therefore, dietary potassium intake, in addition to the sodium to potassium ratio, may play a crucial role in the development of those diseases typically associated with a simple excess of sodium in the modern diet.
Evidence about human salt consumption
The human body has adapted complex physiological mechanisms in order to prevent blood pressure fluctuations in response to these variations in sodium intake. Not surprisingly, epidemiological data has revealed an average sodium intake range of 2400 mg to 5175 mg of sodium per day in developed cultures. Certain isolated groups in areas such as Brazil, Papua New Guinea, and rural African communities have been found to live on sodium intakes of as little as 1150 mg per day. However, despite finding generally low blood pressure in these remote communities, the little evidence that exists on these low salt societies suggests shorter life expectancy and higher mortality rates.
An example from the Intersalt Study, which examined the impact of population-wide salt consumption on blood pressure, is the Yanomami Indians of the Brazilian rainforest, who are known for having far lower average blood pressure than that of Western populations. Their lifelong low blood pressure has been attributed to their extremely low consumption of salt, and this has been used as evidence to further support the effort to restrict salt from the American diet.
A major problem that arises from using the Yanomami as an example of the salt-hypertension hypothesis is the wide variety of confounding variables that may also affect their blood pressure. The Intersalt Study researchers admit that:
“In addition to low Na+ intake and high K+ intake, other factors that may contribute to the absence of hypertension and lack of blood pressure increase with age among the Yanomami Indians are as follows: their low body mass index and the almost nonexistence of obesity, no alcohol ingestion, low ingestion of saturated fat, high ingestion of fibres, relatively high physical activity, and the several cultural consequences of living in an isolated community without the psychosocial stress of civilization and without a monetary system or dependence on a job.”
This data suggests there are many reasons the Yanomami have such low blood pressure. These include high potassium intake, high physical activity, low stress levels, and complete lack of alcohol consumption. Furthermore, although the Yanomami have low blood pressure and nearly non-existent rates of cardiovascular disease, their overall health outcomes are less than stellar. They are described in ethnographic literature as having small stature, high mortality and a low life expectancy ranging between 29 and 46 years. Despite these high mortality rates and confounding lifestyle factors, the Yanomami people are still used as a prime example in support of the salt-hypertension hypothesis.
The results of the Intersalt Study did not indicate any clear pattern between the level of salt intake and blood pressure in those countries studied. And when average life expectancy is plotted against the countries’ average salt intake, the trend shows that higher salt consumption is actually correlated with longer life expectancy. While this correlation does not imply causation, it is interesting to note the compatibility of a high salt diet with a long life expectancy.
As we can see, there is an enormous range in the daily dietary sodium intake of various cultures around the world, ranging from quite low (1150 mg) to fairly high (5175 mg). Additionally, we know that the healthy kidney is capable of adjusting to fluctuating levels of sodium in the diet in order to maintain fluid homeostasis. Finally, we know that hunter-gatherer and Palaeolithic diets were very low in sodium, and that salt was rarely, if ever, added to food. Therefore, it would seem that limiting salt in the diet to those levels recommended by the AHA and USDA would not have any significant consequences, and would be an ideal dietary choice when mimicking the diet of our ancestors. However, evidence is mounting to the contrary: a low-salt diet may actually lead to serious health consequences and higher overall mortality, particularly in conditions like heart disease and diabetes.
The Dangers of Salt Restriction
“In an era when dietary advice is dispensed freely by virtually everyone from public health officials to personal trainers, well-meaning relatives, and strangers on check-out lines, one recommendation has rung through three decades with the indisputable force of gospel: Eat less salt and you will lower your blood pressure and live a longer, healthier life.” Gary Taubes, 1998
Many proponents of the Paleo diet suggest limiting salt based on evidence of low salt intake during the Palaeolithic era. This limitation meshes with recommendations made by various health organizations, such as the USDA and the American Heart Association, who suggest limiting sodium to at least 2,300 mg per day and even as little as 1,500 mg per day. And if our Palaeolithic ancestors ate a low salt diet, then it certainly must be healthy, right?
Not necessarily. Recently, evidence has been mounting against universal salt restriction guidelines. A low-salt diet may cause serious health consequences and higher overall mortality, especially in the presence of certain chronic health conditions and lifestyle factors. In this article, I will discuss scientific evidence that contradicts salt restriction recommendations, as well as potential health risks of consuming a diet too low in salt.
Serious health consequences of long-term salt restriction
While salt-induced hypertension is typically blamed as a cause of heart disease, a low salt intake is associated with higher mortality from cardiovascular events. A 2011 study in the Journal of the American Medical Association demonstrates a low-salt zone where stroke, heart attack and death are more likely. (3) Compared with moderate sodium excretion, there was an association between low sodium excretion and cardiovascular (CVD) death and hospitalization for coronary heart failure. These findings demonstrate the lowest risk of death for sodium excretion between 4 and 5.99 grams per day. (See Figure 1.)
Another 2011 study confirmed this observation; not only was lower sodium excretion associated with higher CVD mortality, but baseline sodium excretion did not predict the incidence of hypertension, and any associations between systolic pressure and sodium excretion did not translate into less morbidity or improved survival.
Low salt diets contribute to an increase in hormones and lipids in the blood. A 2012 study in the American Journal of Hypertension found that people on low-salt diets developed higher plasma levels of renin, cholesterol, and triglycerides. The authors concluded that the slight reduction in blood pressure was overshadowed by these antagonistic effects, and that sodium restriction may have net negative effects at a population level.
In addition, low sodium intake is associated with poor outcomes in Type 2 diabetes. A 2011 study showed people with Type 2 diabetes are more likely to die prematurely on a low-salt diet, due to higher all-cause and cardiovascular mortality. Additionally, a 2010 Harvard study linked low-salt diets to an immediate onset of insulin resistance, a precursor to Type 2 Diabetes. These studies call into question the appropriateness of guidelines advocating salt restriction for patients with Type 2 diabetes.
Restricting salt is also problematic for athletes, particularly those participating in endurance sports. Recent studies have shown that endurance athletes commonly develop low blood sodium, or hyponatremia, even in the absence of cognitive symptoms. In the 2002 Boston Marathon, it was found that 13% of 488 runners studied had hyponatremia, and studies of other endurance events have reported the incidence of hyponatremia to be up to 29%. While the majority of these sodium deficient athletes are asymptomatic or mildly symptomatic with nausea and lethargy, severe manifestations such as cerebral oedema, non-cardiogenic pulmonary oedema, and death can occur. It is extremely important that athletes engaging in high intensity or long duration exercise be sure they adequately replace the salt lost through sweat.
Salt restriction may be especially dangerous for the elderly. Elderly people with hyponatremia have more falls and broken hips and a decrease in cognitive abilities. Hyponatremia is a common finding in the elderly, with an especially high prevalence in those with acute illness. This is another population at risk for serious health consequences due to universal sodium restriction.
Why is the government still recommending salt restriction?
Conventional healthcare experts have been recommending salt restriction ever since the 1970s, when Lewis Dahl established “proof” that salt causes hypertension. In his research, he induced high blood pressure in rats by feeding them the human equivalent of over 500 grams of sodium a day; 50 times more than the average intake in the western world. Dahl also invoked evidence that cultures consuming higher levels of salt tend to have higher blood pressure than those who consume less salt.
See Figure 2. Correlation of average daily salt (NaCl) intakes with prevalence of hypertension in different geographic areas and among different races, from Dahl, 2005
However, when Intersalt researchers investigated this possible association, while controlling for confounding factors, the correlation between blood pressure and salt intake almost disappeared. For some reason, this contradictory evidence is still being used today to justify restricting salt intake.
In 1998, Gary Taubes wrote an article for Science magazine highlighting the clash of public policy with controversial scientific evidence for salt reduction. He described how most of scientific discord over salt reduction has been overshadowed by the public attention given to the benefits of avoiding salt.
As Taubes explained over a decade ago, “the data supporting universal salt reduction have never been compelling, nor has it ever been demonstrated that such a program would not have unforeseen negative side effects.” The 1988 Intersalt Study, designed to resolve contradictions in ecological and epidemiological studies, failed to demonstrate any linear relationship between salt intake and blood pressure. Now, in 2012, we have data that suggests long-term salt restriction may pose serious risks for much of the population. Yet major health organization guidelines still recommend the restriction of salt for all Americans, regardless of blood pressure status.
In short, there is a healthy range of salt consumption for most people. When eating a whole foods diet, most people tend to consume an appropriate amount of salt simply due to an innate preference for saltiness. In fact, the consumption of salt around the world for over two centuries has remained in the range of 1.5 to three teaspoons per day, which appears to hold the lowest risk for disease.
Our bodies may have a natural sodium appetite through which our ideal salt intake is regulated. By following a whole food diet and eliminating processed foods, excess sodium in your diet will be drastically reduced. Thus, you can be confident in following your own natural taste for salt when adding it to your food during preparation. In other words, there are few reasons to deprive yourself of salt
When Salt Reduction May Be Warranted
As we have discussed in the last three articles in my series on salt, the evidence for universal salt reduction is weak and often conflicted. Across different cultures, dietary salt intake is at best weakly correlated with blood pressure or cardiovascular risks, and associated with poorer health outcomes at either extreme of salt intake, both low and high. As a general recommendation, it seems that salt restriction for most people may be both unnecessary and possibly harmful in the long run.
While most people have no reason to restrict salt to the levels recommended by various health organizations, there are a few health conditions in which lower salt consumption may be necessary, based on clinical and population data. Generally, these are people with serious health problems, particularly suboptimal kidney function, and the data supporting salt restriction in these individuals is somewhat controversial.
Salt intake with impaired renal function
For those who have high blood pressure, there is evidence that some hypertensive individuals have inherited salt sensitivity, thought to be caused primarily by impaired sodium transport in the kidney. Our understanding of the salt-sensitivity mechanisms is still underdeveloped, but we do know that certain individuals are far more sensitive to fluctuations in dietary salt. Those individuals with this trait will have a significant blood pressure response to a high salt intake, and would likely benefit from reducing their intake of salt. However, it is thought that potassium intake can greatly impact these effects, and may even eliminate salt sensitivity symptoms. In fact, salt sensitivity is dose-dependently suppressed when dietary potassium is increased within its normal range, so these individuals may benefit more from including ample potassium rather than limiting sodium.
Though the evidence is mixed, patients with chronic renal disease may have better outcomes consuming a lower amount of salt. Those with impaired kidney function typically have reduced glomerular filtration rates and may have more difficulty excreting high levels of sodium. It’s possible that increased dietary salt exposure is toxic to the kidneys when sodium filtration is impaired, and may lead to unsafe levels of proteinuria. These patients need to be cautious about the amount of salt in their diet, though this is a highly individual situation, and largely depends on the type and severity of kidney disease.
High sodium intake may cause excess calcium excretion. Additionally, those who are prone to kidney stones may need to reduce their salt intake, as high sodium excretion also leads to a higher level of calcium excretion in the urine. Again, evidence on this topic is mixed, but it has been demonstrated that excess sodium intake is associated with increased urinary excretion of sodium and calcium, and subjects who consumed the highest levels of sodium tended to have the greatest urinary calcium excretion. Higher calcium excretion may lead to kidney stone formation, particularly if fluid intake is inadequate.
Because of this increased calcium excretion with higher sodium intake, those with osteoporosis may benefit from a lower salt intake as well. Increased losses of calcium in the urine, particularly in the context of low dietary calcium, could be problematic for those at risk for low bone density. However, a high salt intake is not believed to cause osteoporosis, and the potential osteoporotic effects of a high salt intake can be offset by an adequate intake of calcium and potassium.
Of course, it’s important to remember that the majority of these studies have been conducted on subjects consuming the standard American diet of sodium-laden processed food with a heavy emphasis on grains and a deficit of many important vitamins and minerals that we know play significant roles in hypertension, cardiovascular disease, and kidney health. If these sodium studies were conducted in a population consuming a nutrient dense Paleo-type diet,(DBM COMMENT – or even a Whole Food Plant Based Diet) it’s possible the negative effects associated with a high sodium intake would be negligible. As we’ve seen, many of the cultures eating the highest levels of salt have less incidence of cardiovascular disease, kidney disease, and osteoporosis than Americans do. There is evidence that adequate consumption of other minerals may be far more important in blood pressure regulation and other related health outcomes.
Other minerals important for controlling blood pressure
There has been much research into the other dietary minerals that may play a role in blood pressure. The evidence has been mixed on whether certain minerals, particularly supplemental minerals, reduce blood pressure or risk for cardiovascular disease. However, epidemiological and anthropological data suggest that a diet high in certain minerals, such as potassium, magnesium, and calcium, may be beneficial in reducing high blood pressure.
Potassium is likely far more important than sodium intake in the control of blood pressure, as well as reducing the risk of hypertension, kidney stones and osteoporosis. It is believed that human biological machinery evolved to process dietary potassium in amounts many times those of sodium, as Palaeolithic man consumed an estimated 10500 mg of potassium each day, compared to a current US intake of 2500 mg. Therefore, the sodium-potassium ratio of the modern diet is hugely mismatched to our genetically determined renal processing machinery. Additionally, the cardio-protective effects of a relatively high potassium intake have been hypothesized as a basis for low CVD rates in populations consuming primitive diets, where hypertension has been shown to affect only 1% of the population.
Research suggests that increased intake of potassium, found in fruits and vegetables, may be more effective than, and possibly synergistic with, moderately restricting dietary NaCl in reducing not only the renal excretion of calcium, but also the level of blood pressure, the expression of hypertension, and the development of osteoporosis and kidney stones. Therefore, a diet high in potassium-rich plant foods is crucial to preventing the negative outcomes typically associated with a high salt intake.
Magnesium has also been studied for its potential effects on blood pressure, which are poorly understood. Epidemiological studies have typically shown an inverse relationship between dietary magnesium intake and blood pressure, however data from clinical studies have been less convincing of magnesium’s role in treating hypertension. Despite this conflicting evidence, some studies have shown that intracellular magnesium deficiency affects insulin resistance, alters vascular tone leading to hypertension, and induces pro-inflammatory changes and endothelial dysfunction, ultimately increasing the risk for CVD. Therefore, a diet high in magnesium is likely beneficial for anyone at risk for hypertension or heart disease.
Calcium is another major mineral thought to play a role in blood pressure management. A high dietary intake of calcium, but not calcium supplementation, has been associated with both a decrease in blood pressure and the risk of developing hypertension. In fact, calcium supplementation has been associated with a 30% increased risk of heart attack, and is potentially dangerous for those at risk for heart disease. For those looking to protect themselves against hypertension and subsequent cardiovascular disease, a calcium-rich diet should suffice, with no supplementation required or recommended. (And of course, remember to keep vitamin K2 intake adequate as well!)
Take home message? Use your own judgment!
Ultimately, the amount of salt required for good health is based on individual needs, health status, and genetic predisposition to salt sensitivity. The evidence for salt restriction, even for those with cardiovascular or renal disease, is mixed and often times inconclusive. It’s important to remember that the data regarding sodium intake has been from populations typically eating a standard American diet, and it’s unknown whether salt intake would demonstrate any detrimental effects in a population eating a potassium, magnesium, and calcium rich whole foods diet. These are important points to consider when deciding how much salt to include in your own diet.
How much, and what kind of salt to include in the diet
According to research, there exists a range of sodium intake that likely confers the best health outcomes for most people. As I explained in part 3, findings from a 2011 study demonstrate the lowest risk of death for sodium excretion between 4000 and 5990 milligrams per day. Sodium excretion greater than 7000 milligrams or less than 3000 milligrams per day was associated with a higher risk of stroke, heart attack and death. This lowest risk range equates to approximately two to three teaspoons of salt per day.
See: Figure 3: Mean sodium intake among the participants of the Japanese National Nutrition Survey: 1973–2000
The average American consumes about 3700 milligrams of sodium a day. This value has remained constant for the last fifty years, despite the rise in rates of high blood pressure and heart disease. As a comparison, the Japanese, with one of the highest life expectancies in the world, consume an average of 4650 milligrams of sodium per day, and have a lower risk of cardiovascular disease than most other developed countries. Their average sodium intake has consistently hovered in the low risk range over the past 30 years, despite attempts by public health organizations to reduce Japanese salt consumption. A caveat is that the Japanese also have a high risk of stroke, so their extremely high salt intake is not necessarily recommended as a model for our own intake.
While salt recommendations vary between individuals based on age, gender, physical activity, and health conditions, I feel that the data supports an intake between 3000 and 7000 milligrams of sodium, or 1.5 to 3.5 teaspoons of salt, per day. People who are quite active or sweat a lot should consume salt on the higher end, and those who are less active may want to consume on the lower end. Of course, there may be some conditions where moderate salt restriction is warranted, but for the majority of healthy individuals, salting to taste will provide an appropriate level of sodium in the diet. Natural sources of sodium include sea vegetables, fish, shellfish, and meat, plus certain plants such as beets, carrots, celery, spinach, and turnips.
Article Source: Chris Kresser, follow the link to see the original article and the references attached to it.